WHAT IS AN ABDOMINAL AORTIC ANEURYSM?
WHAT IS AN ABDOMINAL AORTIC ANEURYSM?
The term abdominal may lead you to believe that this aneurysm is in your stomach, but aortic aneurysm commonly occurs in the aorta immediately below the kidneys but above the iliac arteries going to the legs.
The aorta is the main trunk of the arterial system. It carries oxygenated blood from the heart to the body.
An aneurysm is an abnormal widening of an artery, in this case the aorta. This means that the artery stretches to more than 1.5 times its normal diameter. As blood pumps through, this stretching weakens the artery’s wall, often creating an egg-shaped ballooning.
An aneurysm can occur in any blood vessel, but most commonly occurs in the aorta. Treatment of Abdominal Aortic Aneurysm often requires surgery and medication, but your treatment depends greatly on your individual situation. The smaller your aneurysm, the less immediate risk it presents. The goal of treatment is to avoid having the aneurysm rupture. Our report outlines the benefits and risks of your possible treatment options.
Abdominal Aortic Aneurysm can affect anybody, but most often affects men between 40 and 70. Abdominal Aortic Aneurysms occur in 5 to 7% of people older than 60 in the United States, but children can develop it as a result of trauma or illness.
WATCHFUL WAITING
The physician may recommend “watchful waiting”, which means that the patient has to be monitored every 6 months for signs of changes in the aneurysm. The physician may schedule you for regular CT scans or ultrasounds to watch the aneurysm. This method is usually used for aneurysms that are smaller than about 2 inches (or 5.0 – 5.5 centimeters). If the patient has high blood pressure, the physician may prescribe blood pressure medication to lower your blood pressure and lower the pressure on the weakened area of the aneurysm.
An aneurysm will not “go away” by itself. It is extremely important to continue to follow up by a vascular specialist as directed because the aneurysm may enlarge to a dangerous size over time and could eventually burst.
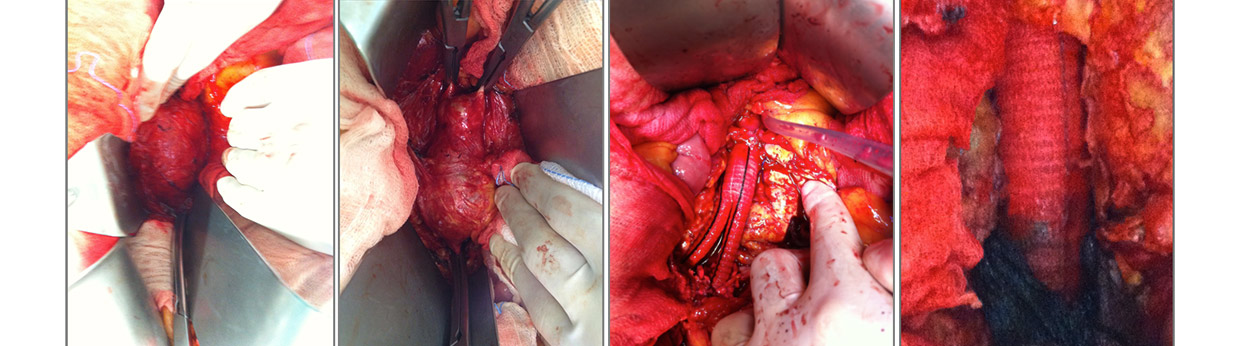
OPEN SURGICAL ANEURYSM REPAIR
A vascular surgeon may recommend for a surgical procedure called open aneurysm repair if the aneurysm is causing symptoms or is larger than about 2 inches (or 5.0 to 5.5 centimeters), or is enlarging under observation. During an open aneurysm repair, also known as surgical aneurysm repair, the surgeon makes an incision in the abdomen and replaces the weakened part of your aorta with a tube-like replacement called an aortic graft. This graft is made of strong man-made material, such as plastic, in the size and shape of the healthy aorta. The strong tube takes the place of the weakened section of the aorta and allows the blood to pass easily through it.
Following the surgery, you may stay in the hospital for 5 to 10 days. The patient may also require 2 to 3 months for a complete recovery. More than 90 percent of open aneurysm repairs are successful for the long term. A stroke occurs when the blood flow to the brain is interrupted resulting in a loss of nutrients and oxygen. If the blood flow is not restored the brain cells die and there will be permanent brain damage. Stroke is a major cause of disability and death. Carotid stenosis is one of the many causes of stroke.
ENDOVASCULAR STENT GRAFT
Endovascular means that the treatment is performed inside your body using long, thin tubes called catheters that are threaded through your blood vessels. This procedure is less invasive, meaning that the surgeon will need to make only small incisions in your groin area through which to thread the catheters. During the procedure, the surgeon will use live x-ray pictures on a video screen to guide a fabric and metal tube, called an endovascular stent graft (or endograft), to the site of the aneurysm. Like the graft in open surgery, the endovascular stent graft also strengthens the aorta.
The recovery time for endovascular stent graft is usually shorter than the open surgery, and the hospital stay may be reduced to 2 to 3 days. However, this procedure requires more frequent imaging procedures after placement to be sure the graft continues to function properly, and is more likely to require periodic maintenance than the open procedure. Not all patients are candidates for endovascular repair because of the extent of the aneurysm, its relationship to the renal (kidney) arteries, or other issues. While the endovascular stent graft may be a good option for some patients, in some other cases, open aneurysm repair may still be the best way to cure AAA.
VIEW AN ABDOMINAL AORTIC ANEURYSM
WHAT IS CAROTID STENOSIS?
Carotid stenosis refers to the blockage and narrowing of the carotid artery in the neck. The Carotid artery supplies blood to the brain fig.8,9. This blockage is causes by fatty build up called plaque and is also referred to as atherosclerosis. This fatty material accumulates in the inner lining of blood vessels and results in narrowing, stenosis and irregularity of the artery. This may result in the formation of blood clots which dislodge and flow up to the brain.
A stroke occurs when the blood flow to the brain is interrupted resulting in a loss of nutrients and oxygen. If the blood flow is not restored the brain cells die and there will be permanent brain damage. Stroke is a major cause of disability and death. Carotid stenosis is one of the many causes of stroke.
WHAT CAUSES IT?
There are many risk factors associated with carotid stenosis:
1. Age, the older you are the higher the risk.
2. High blood pressure. This should be treated and maintained below 140/90.
3. Smoking. This increases the risk of carotid stenosis and stroke.
4. High cholesterol levels. High blood levels specifically of LDL can accelerate development of carotid stenosis.
5. Diabetes or high blood sugar.
6. Obesity. This increases the risk of high blood pressure as well as increases the development of atherosclerosis.
WHAT ARE THE SYMPTOMS?
The exact symptoms depend on the area of the brain affected, although many patients are asymptomatic and the stenosis is discovered on clinical exam. Patients may present with a transient ischemic attack (TIA). This cerebrovascular event lasts seconds to hours, but less than 24 hours. This temporary blockage of the blood vessel may cause momentary loss of vision in one eye, weakness/numbness of one side of the body, slurred speech or an inability to get words out. It is important to consult a physician immediately as this may lead to a major stroke.
HOW IS THIS DIAGNOSED AND TREATED?
A physician may be able to hear a noise over the carotid artery with a stethoscope. This noise is called a carotid bruit and is made by blood flowing past an area of turbulence. Some other diagnostic tests include: Doppler Ultrasound. This noninvasive test uses ultrasound waves to reconstruct an image of the carotid arteries and the blood flow through the arteries. MRI/MRA. These tests use magnetic fields to generate an image. Angiography. test is currently considered the ‘gold standard’, but involves some risk. Pictures are taken of the blood vessel while a dye is injected.
This carotid stenosis may not cause any symptoms at call and therefore treatment indications for asymptomatic stenosis are less firm than for symptomatic stenosis.
VIEW A CAROTID ENDOARTERIECTOMY
HOW IS THIS TREATED?
Treatment of carotid artery disease usually involves a combination of lifestyle changes, medication and sometimes surgery.
In carotid endarterectomy, you receive a local or general anesthetic. Your surgeon makes an incision along the front of your neck, opens your carotid artery and removes the plaques that are clogging your artery. Your surgeon then repairs the artery with stitches or a patch made with a vein or artificial material (patch graft).
Sometimes surgeons may use another technique called eversion carotid endarterectomy, in which the carotid artery is cut and turned inside out and the plaque removed. Your surgeon then reattaches the artery.
Doctors may recommend carotid endarterectomy if you have more than 60 percent blockage in your arteries. You may or may not be experiencing symptoms. Your doctor will evaluate your condition and determine whether you’re a candidate for carotid endarterectomy.
Doctors may determine you’re a candidate for a procedure called carotid angioplasty and stenting instead of carotid endarterectomy. In this procedure, doctors thread a thin tube (catheter) with a small balloon attached through a blood vessel in your neck to the narrowed artery. The balloon is then inflated to widen the artery and a small wire mesh coil (stent) is often inserted to keep the artery from narrowing again.